Which Of The Following Statements About The First Step Of The Line Drawing Technique Are Incorrect
This commodity, the second in a 4-part serial, describes the procedure for collecting a catheter specimen of urine
Citation:Shepherd E (2017) Specimen collection 2: obtaining a catheter specimen of urine. Nursing Times [online]; 113, 8, 29-31.
Author:Eileen Shepherd is clinical editor at Nursing Times.
- This article has been double-blind peer reviewed
- Coil downwards to read the article or download a print-friendly PDF hither
- Click hither to run into other articles in this series
Introduction
Obtaining a specimen involves collecting tissue or fluids for laboratory analysis or near-patient testing, and may be a kickoff step in determining a diagnosis and treatment (Dougherty and Lister, 2022). Specimens must exist nerveless at the right time, using the right technique and equipment, and exist delivered to the laboratory in a timely way (Dougherty and Lister, 2022). Box i provides a reminder of the general principles of specimen collection, which were discussed in more particular in part ane (Shepherd, 2022).
Box 1. Professional issues and adept do principles
Nurses must:
- Be aware of their organisation'due south policies and procedures for specimen collection
- Be able to explain the purpose of the specimen to the patient and the implications for treatment, and to obtain informed consent
- Be competent to undertake the procedure (NMC, 2022). This includes cognition of correct procedure for drove, handling and transportation of the sample (Dougherty and Lister, 2022)
- Be aware of infection prevention and control principles involved in collection of tissue and body fluids (Loveday et al, 2022)
- Understand the importance of accurate record keeping. Documentation should include fourth dimension the specimen was collected, results and changes to handling that occur in response to the results (Dougherty and Lister, 2022)
The specimen must exist:
- Appropriate to the patient's clinical presentation
- Collected at the right fourth dimension
- Nerveless in a way that minimises the take a chance of contamination
- Collected in a manner that reduces risk to all staff (including laboratory staff)
- Collected using the right equipment
- Documented conspicuously
- Stored/transported accordingly (Higgins, 2008)
The collection of whatever tissue/fluid carries a gamble to staff from splash or inoculation injury, then standard precautions should be followed (Loveday, 2022).
Indwelling urinary catheters
Indwelling urinary catheterisation involves the insertion of a tube into the float using aseptic technique (Dougherty and Lister, 2022).
The process is carried out on patients for a diversity of reasons, including to:
- Manage acute and chronic urinary retention;
- Accurately measure urine output in acutely ill patients;
- Featherbed an obstruction such every bit an enlarged prostate gland in men;
- Administer drugs directly into the bladder and deport out bladder function tests (Yates, 2022a).
Catheters tin as well exist used to manage incontinence and maintain skin integrity when all other conservative direction strategies accept been attempted and failed (Dougherty and Lister, 2022; Royal College of Nursing, 2022).
Indwelling urinary catheterisation is associated with a number of complications, including:
- Catheter-associated urinary tract infection (CAUTI);
- Tissue harm;
- Bypassing and blockage (Yates, 2022a).
As there is a adventure of complications, catheters should be used only when no alternatives are appropriate. Catheters should also be removed as soon as clinically appropriate (Loveday et al, 2022).
Catheter specimen of urine
Catheter specimens of urine (CSU) are usually collected for microscopy, culture and sensitivity (MC&S) testing when an infection has been suspected. The urine is tested to identify the organisms causing the infection as well as their sensitivities to antibiotics.
A CSU should only be collected when a patient has clinical signs of a CAUTI (Box 2). The decision should not be based solely on the sight or smell of urine in the drainage bag equally these are non good indicators of infection in catheterised patients (Scottish Intercollegiate Guidelines Network, 2022).
Box 2. Clinical signs of CAUTI
- Fever
- Rigor, shivering, shaking
- New onset or worsening defoliation/delirium
- Lethargy with no other identified cause
- Back pain/pelvic pain
- Acute haematuria
Source: SIGN, 2022
Principles of specimen drove
Indwelling urinary catheters are usually attached to a drainage handbag to create a airtight drainage organization. Breaking this airtight system – for example by disconnecting the catheter from the drainage device or emptying the drainage pocketbook, can increase the take a chance of CAUTI (Loveday et al, 2022).
Some patients have a catheter valve in place instead of a drainage bag, which allows the bladder to fill and and then requires the patient (or a health professional or carer) to release the valve and allow the bladder to empty. Using the catheter valve helps maintain bladder tone and can be the method of choice for some patients. For further information on catheter valves run across Yates (2017b).
A fresh sample of urine is required for a CSU and this must be obtained from the sampling port on the catheter bag or in the instance of a catheter valve, straight from the valve. The sampling ports are designed to be accessed directly using a syringe and do not crave a needle, therefore removing the risk of sharps injury (Dougherty and Lister, 2022).
Samples should not exist nerveless from the drainage bag tap as the urine specimen may be contaminated (Brekle, 2022) and inaccurate results may atomic number 82 to inappropriate handling. Ideally, samples should be collected earlier antibiotics are commenced every bit they may affect the result of the laboratory investigation.
Equipment
The following equipment is required:
- Clean tray to concord equipment;
- Non-sterile gloves;
- Apron;
- Sterile 10ml syringe (not required if taking a specimen from a catheter valve);
- Non-traumatic clamp (not required if taking a specimen from a catheter valve);
- Specimen container;
- Alcohol-impregnated swabs (two% chlorhexidine in 70% isopropyl alcohol);
- Sterile jug (if taking a CSU from a catheter valve);
- Documentation and forms.
The process
Collecting from a sampling port
An aseptic non-impact technique (ANTT) must be used to obtain a CSU equally this reduces the risk of cross infection (Rowley, 2022).
- Decontaminate hands and prepare the equipment.
- Explain the procedure to the patient and gain informed consent to obtain the specimen. Information technology is important to explain why the specimen is being collected, when the results will be bachelor and implications for handling (Dougherty and Lister, 2022).
- Ensure the patient is comfy and that their privacy and nobility is maintained throughout the procedure.
- Decontaminate your hands and put on an frock.
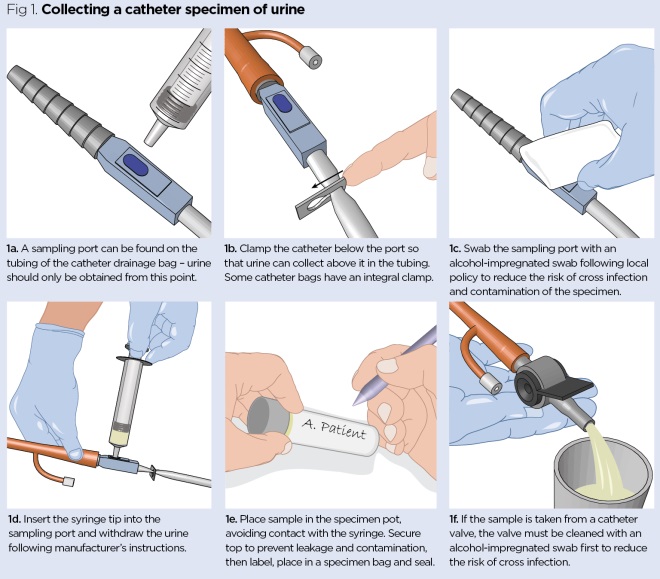
- If taking a specimen from a sampling port (Fig 1a), check first whether there is urine in the catheter tubing. If the tubing is empty use a clench below the level of the sampling port (Fig 1b). This allows urine to collect to a higher place the clench then that a sample tin be obtained.
- Decontaminate your hands and employ not-sterile gloves. Clean the sampling port with an alcohol-impregnated swab according to local policy and permit to dry out (Fig 1c). This reduces the gamble of cross infection or contagion of the specimen (Rowley, 2022).
- Stabilise the tubing past holding it beneath the level of the sampling port.
- Insert the syringe tip into the sampling port (post-obit manufacturer'due south instructions) (Fig 1d). Be careful to protect the sterile syringe tip and disinfected sample port from contagion.
- Aspirate at least 10ml of urine and withdraw the syringe.
- Put the urine into a sterile universal container, fugitive contact between the syringe and the pot (Fig 1e). Ensure the height of the specimen container is secured to prevent leakage and contamination of the specimen.
- Wipe the sampling port with an booze-impregnated swab and permit to dry. This reduces the risk of cross infection and contamination (Dougherty and Lister, 2022).
- If a clamp was used, release information technology to let urine drainage freely. Failure to exercise this will cause the bladder to make full and can result in discomfort and bypassing of urine around the catheter, which can be distressing for the patient.
- Remove and dispose of gloves and apron, and launder hands with soap and water.
- Complete the asking form, label the specimen and place in a specimen handbag post-obit local policies.
- Send the sample to the laboratory immediately or refrigerate until it tin can be transported to ensure accurate results are obtained (Dougherty and Lister, 2022).
- Certificate the date and time the sample was collected in the patient'southward notes.
Collecting from a catheter valve
First, follow steps i-4 above and and then:
- Ensure the patient has a full bladder.
- Apply not-sterile gloves and clean the catheter valve port with an alcohol-impregnated swab co-ordinate to local policy and permit to dry out. This reduces the adventure of cross infection (Fig 1f).
- Open the valve and release a small amount of urine to affluent the valve.
- Open up the valve over again and empty the remaining urine into a sterile jug, ensuring the valve does not come into direct contact with the jug.
- Put a sample of urine in a sterile universal container. Ensure the elevation of the specimen container is secured to foreclose leakage and any contamination of the specimen.
- Close off the valve and wipe the port with an booze-impregnated swab.
- Dispose of any remaining urine according to local policy.
- Follow steps 13-16 above to complete the procedure.
Professional responsibilities
This procedure should be undertaken only afterward approved training, supervised practice and competency assessment, and carried out in accordance with local policies and protocols.
Brekle B (2014) Specimen drove - microbiology and virology.
Dougherty Fifty, Lister Due south (2015) The Purple Marsden Hospital Manual of Clinical Nursing Procedures. Oxford: Wiley-Blackwell.
Higgins D (2008) Specimen collection 1. obtaining a midstream specimen of urine.Nursing Times; 104: 5, 26-27.
Loveday HP et al (2014) epic3: national evidence-based guidelines for preventing healthcare-2associated infections in NHS hospitals in England. Journal of Hospital Infection; 86: S1, S1–S70.
Rowley S (2011) ANTT: A standard approach to aseptic technique. Nursing Times; 107: 36, 12-14.
Scottish Intercollegiate Guidelines Network (2015) Direction of Suspected Bacterial Urinary Tract Infection in Adults.
Shepherd E (2017) Specimen collection i: general principles and procedure for obtaining a midstream urine specimen. Nursing Times; 113; vii, 45-47.
Yates A (2017a) Urinary catheters 5: teaching patients how to apply a catheter valve. Nursing Times; 113: 5, 25-27.
Yates A (2017b) Urinary catheters 1: male person catheterisation. Nursing Times; 113: one, 32-34.
Source: https://www.nursingtimes.net/clinical-archive/assessment-skills/specimen-collection-2-obtaining-a-catheter-specimen-of-urine-10-07-2017/
Posted by: billupsthavite.blogspot.com


0 Response to "Which Of The Following Statements About The First Step Of The Line Drawing Technique Are Incorrect"
Post a Comment